The wisdom of the pulse wave: The arterial flow resistance
Arterial flow resistance is a guiding parameter that provides more accurate insights into individual vascular health than conventional metrics.
The arterial flow resistance
The wisdom of the pulse wave
The arterial flow resistance of the major conduit arteries is a relatively unknown parameter to date and thus widely underestimated. In our opinion, however, it represents the most significant parameter of all — because it acts as indicator easy to comprehend when it comes to the patency of major conduit arteries. This gives it far greater significance than vascular stiffness, which is usually given preferential consideration. Interestingly, arterial flow resistance does not always correlate with vascular stiffness when measured.
Until now, arterial flow resistance has been very difficult to measure both directly and indirectly by conventional means. This is where Model-based Pulse Wave Analysis (mbPWA) makes its appearance, by far exceeding any other diagnostic approach: The underlying measurement principle is based on the individually determined vascular data of the arterial tree of any patient. Drawing on an algorithmically generated “vascular avatar”, arterial flow resistance can now be easily and reproducibly be determined for the first time ever: Cardiovascular diagnostics on a completely new level.

The physical context
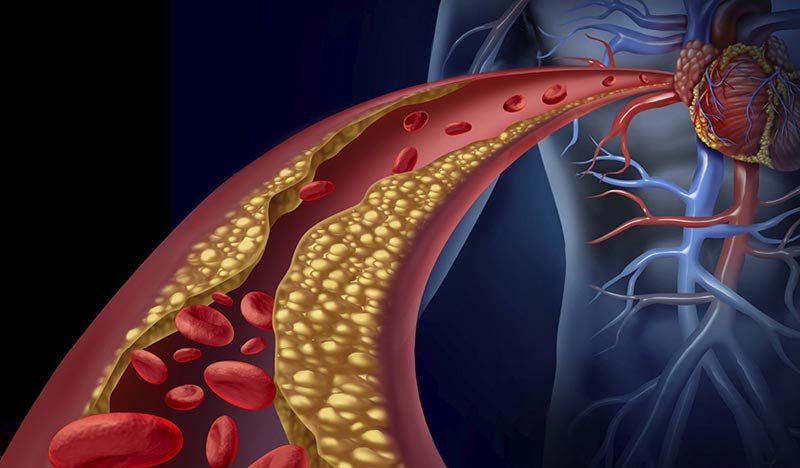
To illustrate, let’s take a look inside the arteries: The arterial flow resistance is influenced by the mean free lumen (the vessel diameter) in its function as conduction resistance. Sometimes plaques form on a particular arterial segment. Plaques are patchy, inflammatory lesions (injuries) of the vessel wall. The underlying causes are varied and have not been fully explored in detail. However, there are known risk factors such as hypertension, diabetes, dyslipidemia, nicotine, and physical inactivity, among others. These factors can severely impair endothelial function, leading to vasoconstriction via several successive processes.
Consequently, in the course of all these ongoing processes, resistance increases due to the now reduced vessel diameter. When the variation of vascular tone, i.e., the ability to dilate or constrict vessels, is limited due to atherosclerosis and the accompanying endothelial dysfunction, resistance increases significantly even at rest. To make matters worse, plaque deposition in the vessels and atherosclerosis often occur together. The result of this fatal combination is that in such severe cases of endothelial damage, resistance increases twice as much. The good news is that this also makes it particularly easy to detect these pathological changes in measurements. Changes in the inner diameter of the arteries are included in the resistance to the fourth degree (!).
The clinical benefit of arterial flow resistance: leading through sensitivity
In some cases, the increase in arterial flow resistance is detectable at the surprisingly young age of 20–30 years — in patients with obesity, for example. This allows for the diagnosis of problematic cardiovascular conditions before they become clinically relevant. In many cases, consequential diseases can then be prevented by ways of early therapeutic interventions and personal initiative in the sense of regular exercise and healthy dietary routines.